Improving patient engagement through shared-decision making
In 2021, Beth Israel Lahey Health and BlueCross BlueShield of Massachusetts began to focus on the idea that doctors and patients should have equal weight in deciding on health-related procedures. It’s a concept known as shared decision making. Research shows that shared decision making supports the notion that if a patient is engaged in their care, they’re more likely to follow through on preventative cancer screenings and improve their own self management of their care.
“We saw this as a win-win for both the patient and the providers, to have that two way conversation on what the patient prefers for their screening, should they decide to get screened. And colorectal cancer screening made sense to us because there are different options to get screened,” said Tim Carey, Clinical Operations Project Manager (Performance Network) at Beth Israel Lahey Health (BILH).
Carey along with Laura Carr, Director, Provider Performance at Blue Cross Blue Shield of Massachusetts (BCBSMA) recently spoke with Nina Zelcer, Senior Manager at Arcadia to explain how shared decision making is a win-win-win for providers, payers, and patients during the webinar, Payer-Provider Collaboration.
Patient engagement through shared decision making
The idea behind shared decision making is motivating the patient to take action and complete their screenings or participate in their care.
“Overall shared decision making is a communication approach to better educate patients so they can make informed decisions in collaboration with their provider,” Carr said.
While some may believe, in the instance of colorectal cancer, a colonoscopy is the only screening option, in reality there are other options and the best test is the test that gets done.
“The whole point of the cancer screening is to detect cancers early to improve patient outcomes. And if the colonoscopy is what the provider is most accustomed to ordering, but that’s not what the patient is going to follow through on, then they’re not going to complete that screening, they’re not going to find that cancer early. So finding the test that fits best for them, so that they can have that screening completed is the aim of all of this work,” she added.
Identifying the right patients for the program
BILH and BCBSMA used the patient data stored on their Arcadia platform to identify the right patients. They set parameters to contact patients within the eligible age range for colorectal cancer screening, 45-75.
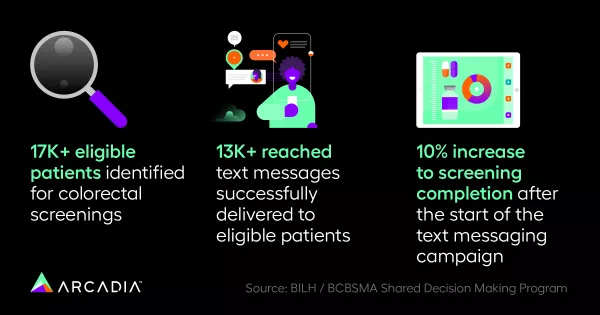
The goal was to reach patients between 45-49 who were new to the screening process and older patients who were not engaging in screenings ahead of their primary care appointments.
Engaging patients in shared decision making through text messaging
BILH and BCBSMA developed a decision aid tool—a pdf document with evidence-based information about the different colorectal cancer screen options—that it could share with patients to involve them in their screening decision.
“We collaborated with our medical and research, academic research teams, our primary care physicians, the specialists, our patient family advisory committee to build a really simple and easy to digest decision aid,” Carey said.
The tool is sent out via text message prior to the patient’s appointment with their provider to discuss during the appointment.
“We’ve been pushing this out, I think, in total it’s definitely over 17,000; it’s closer to 20,000 patients. And we’re seeing great success with that, a 10% increase in the screening completion,” he explained.
The results have been life-saving for some patients.
“We’ve been able to really capture patients that have not had a screening that should have, we’re able to get them screened and, with the proper screening, prevent them from either getting cancer, or complications from cancer if it gets too late stage,” Carey added.
Health equity through multilingual texts
The text messages went out in English, Spanish, and Portuguese and BILH plans to expand the number of languages in which the decision aid is available.

“There is research that shows patient engagement and shared decision making tools do decrease discrepancies in care, and that you can improve the health equity of these quality measures by using shared decision making to engage the patient and make a choice that’s right for them,” said Carr.
Challenges with outreach
One drawback to outreach via text message was age. Patients 49-59 were highly likely to receive the message on their cell phones. However, patients 60-75 the technology often reached a landline that could not receive the message.
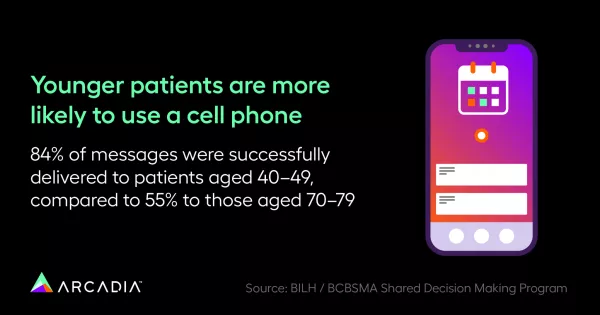
BILH and BCBSMA continue to explore work-arounds for this situation, because it is ideal for patients to receive the information and digest it ahead of their appointments.
Results of BILH and BCBSMA’s program
Over the past year, as more patients were educated about their choices, BILH and BCBSMA saw an increasing number of those screened using the FIT DNA at-home colorectal cancer screening test; from less than 5% to nearly 20%.
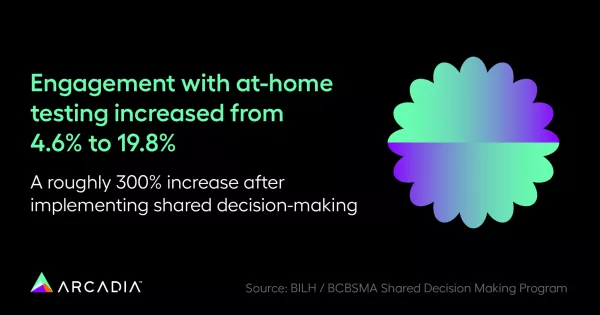
“People are now saying I don’t have to take a day off, I don’t have to do all that prep, I can get a test at home that may be more convenient for me, or maybe from an equity point of view, I can’t take a day off from work, I can’t afford that, or I have no transportation to get a colonoscopy, so the home option is best for them,” Carey explained.
Other results indicated that while fee-for-service providers of colonoscopies might be expected to be upset at a reduced patient load, the reverse was true. The option of a FIT DNA screening has helped them manage the extensive backlog of patients seeking colonoscopies since the pandemic. And, primary care physicians who worried that the added conversation would negatively impact their schedules, found, in practice, the short conversation did not affect them significantly and in fact, will reduce further conversations when patients have a plan they will actually act on.
The future of shared decision making in healthcare
Shared decision making is poised to grow in use. It has the potential to be implemented in many other areas of healthcare. Technology used to identify target patients and deliver messaging to them will increase in options for healthcare organizations; as will patients’ and providers’ comfort in using it.
“It’s really the patient’s life, it’s the patient’s health, having the patient engaged makes them more likely to follow through on their care,” Carr said. “Studies that show engaging a patient in decisions about what medications to use, make them more likely to continue to use those medications, engaging patients in decision making about certain procedures make them more likely to follow through on the procedure.”
Watch the full webinar and reach out to Arcadia to start brainstorming solutions together.



