In 2020, Arcadia’s MSSP ACO customers generated $386M in shared savings, averaging $10.7M each
Since 2013, the company has helped generate a total of over $1 billion in MSSP savings
Burlington, Mass. — Sept. 28, 2021 — Arcadia (arcadia.io), the leading population health management and health intelligence platform, helped its national network of Accountable Care Organizations (ACOs) generate more than $386 million in the 2020 Medicare Shared Savings Program (MSSP) using the company’s population health management platform, Arcadia Analytics.
Key data for the 2020 performance year
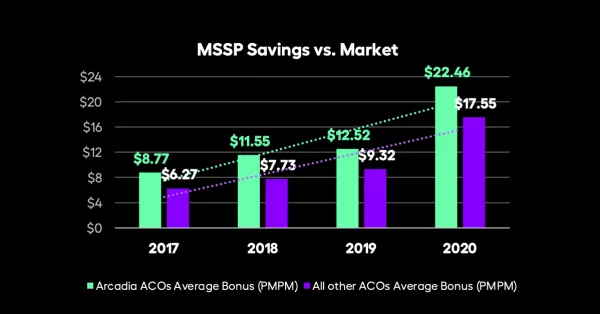
- Arcadia’s MSSP ACO customers outperformed their peers, generating an average gross savings of $10.7 million per customer.
- Average per member per month (PMPM) bonuses were $4.90 higher than those earned by other ACOs.
- Arcadia customers realized an additional $5.63 in PMPM savings when compared to other ACOs.
Health systems’ evolution from fee-for-service to value-based care requires providers to assume greater financial risk while being rewarded for producing positive patient outcomes, making it essential that providers base patient-care decisions on data and evidence. Arcadia Analytics aggregates patient data from disparate sources to enable ACO partners to illuminate key drivers of cost and utilization, measure performance, find and close risk and quality gaps, and identify impactable patients for care management and outreach.
Leveraging these data-driven insights, ACOs achieve better and more sustainable financial outcomes with Arcadia Analytics by combining the most comprehensive patient view with actionable AI-powered insights into care team-centered workflows for outreach, documentation, tasking, and care coordination.
Without aggregated data, analytics and insights, ACOs often have trouble making informed decisions that will improve their performance trends effectively. This steady, year-over-year rise in our customers’ earned savings shows the impact of our Arcadia Analytics platform.
— Sean Carroll, CEO, Arcadia
A Proven Strategy for ACO Success
To improve value-based care strategies and performance, Arcadia’s data and software drives success in complex savings and reimbursement arrangements. Arcadia provides its ACO customers with tactical market expertise, a data asset, and workflow tools to help them reduce total medical expense, increase risk adjustment accuracy, and improve the quality of care.
“Given the difficulties created by the pandemic, 2020 was a very challenging year for the entire healthcare industry. Providers struggled to give patients the care they needed while achieving value in the process,” Carroll said. “We were able to help our ACO customers not only continue with their care delivery strategies, but also improve their performance. We remain very proud of our long-term strategic work with our MSSP ACO customers as they rise to the challenges of delivering value-based care with significant, solid results.”
About the Medicare Shared Savings Program
The largest value-based payment model in the country, the Medicare Shared Savings Program (MSSP) is a voluntary program that requires ACOs to share in losses—or take financial risk—if spending for patient care increases beyond a benchmark target. In 2020, the Centers for Medicare and Medicaid Services waived any shared losses for at-risk ACOs, citing the need for providers to focus on the COVID-19 public health emergency.
About Arcadia
Arcadia is dedicated to happier, healthier days for all. We transform data into powerful insights that deliver results. Through our partnerships with the nation’s leading health systems, payers, and life science companies, we are growing a community of innovation to improve care, maximize value, and confront emerging challenges. For more information, visit arcadia.io.
# # #
