HCC risk suspecting software integrated with Epic for risk adjustment
Arcadia HCC Risk Suspecting App is now available — download product info.
Healthcare providers are dealing with too much data
Diagnosis data typically lives in various systems such as employee health records (EHRs), EHR instances, and payer files. Provider actions taken in one place are not always reflected across these systems. Navigating multiple systems for suspected diagnoses is time-consuming and frustrating and can take away from time spent with patients as well as negatively impact risk adjustment performance.
There is an easier way.
Surface suspect health conditions with risk suspecting software
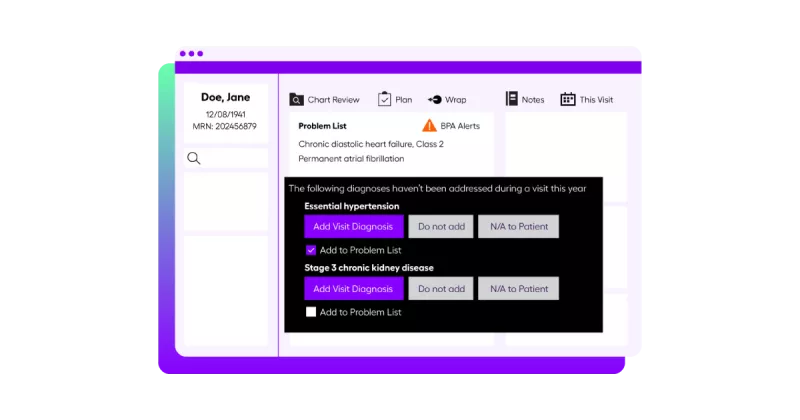
Act on the information that matters most. Surface suspected, historical, and persistent documented conditions at point of care within Epic Best Practice Advisory (BPA) workflows. Providers can address these gaps in-visit, without ever leaving Epic.
The Arcadia HCC Risk Suspecting App gives your providers actionable data within existing Epic workflows to prompt action and drive outcomes.
Increase provider satisfaction and decrease burnout
- Seamlessly incorporate suspected diagnoses from Arcadia natively within the Epic HCC Best Practice Advisory (BPA) workflow
- Reduce workload on front-line providers and avoid duplication of data
Capture disease burden and impact outcomes at scale through suspect HCCs
- Arcadia HCC Risk Suspecting App is built on an integrated payer and EHR data asset, enabling diagnosis suspecting from notes, labs, orders, vitals, and more
- Our centralized risk platform enables a “closed loop” for addressing suspected risk gaps
Complement and maximize your Epic EHR investment
- Our integration is available in Epic
- All this enables providers to meet their goals while minimizing IT overhead and security exposure

Data analytics for population health management
Arcadia aggregates claims, clinical, and ancillary data and enriches the data with a proprietary risk suspecting engine. Diagnosis-level suspected, historical, and persistent documented conditions are surfaced in Epic’s BPA HCC Risk Adjustment workflow via FHIR integration. Suspected diagnoses from Arcadia are automatically written to the Epic problem list, so the clinician only needs to review and reconcile directly within their workflow to generate billable codes.
Learn more about our HCC Risk Suspecting App
Impact outcomes at scale and tap into your existing workflows with the Arcadia HCC Risk Suspecting App without ever leaving Epic — now available in the Epic. Our integration is the ideal way to surface actionable population health insights at point of care.